Clinical Image
Pulmonary Infarction Mimicking An Aspergilloma In A Heart Transplant Recipient

Antonacci F1*, Belliato M2 Bortolotto C3, Di Perna D4, Dore R3, Orlandoni G1 and D’Armini AM4
1Thoracic Surgery, Foundation IRCCS Policlinico San Matteo, Viale Golgi 19, Pavia, Italy
22nd ICU, S.C. Anestesia e Rianimazione 2, Foundation IRCCS Policlinico San Matteo, Pavia, Italy
3Radiology, Foundation IRCCS Policlinico San Matteo, Pavia, Italy
4Cardiac Surgery, Foundation IRCCS Policlinico San Matteo, University of Pavia, Pavia, Italy
*Address for Correspondence: Filippo Antonacci, Thoracic Surgery, Foundation IRCCS Policlinico San Matteo, Viale Golgi 19, Pavia, Italy; Email: [email protected]
Dates: Submitted: 01 January 2017; Approved: 27 January 2017; Published: 30 January 2017
How to cite this article: Antonacci F, Belliato M, Bortolotto C, Di Perna D, Dore R, et al. Pulmonary Infarction Mimicking An Aspergilloma In A Heart Transplant Recipient. J Clin Med Exp Images. 2017; 1: 005-006.
DOI: 10.29328/journal.jcmei.1001002
Copyright License: © 2017 Antonacci et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Pulmonary aspergillosis; Lobectomy; Pulmonary infarction
CASE DESCRIPTION
This patient (male, 59 years old) underwent cardiac re-transplantation for chronic rejection. Prior to re-transplantation, the patient was in NYHA class IV, with a clear chest x ray. On 14th postoperative day, he presented hemoptysis. On chest x-ray, a left lower lobe opacity was seen. Therefore, a chest CT scan was done and it showed a round mass within a pulmonary cavity surrounded by airspace in proximity of the pulmonary artery. The radiologist strongly suspected a pulmonary lesion similar to an aspergillum’s disease. The radiological appearance together with the immunocompromised status of the patient made the diagnosis of aspergillosis possible. Considered the high risk of a devastating hemoptysis due to the aspergillum vascular invasiveness, a left lower lobectomy was performed. The following course was characterized by a difficult weaning from mechanical ventilation and the patient was discharged on 45th postoperative day post lobectomy. Surprisingly pathological examination showed an abscessual cavity in an area of pulmonary infarction.
We focused on aspergillosis in view of the above-mentioned aspects, nevertheless a differential diagnosis of pulmonary infarction could have been considered because of the prolonged bed rest and recent surgery. Lung lobectomy appeared to be the correct treatment since, both in case of aspergilloma and in case of pulmonary infarction, the left inferior lobe would have never recovered a normal function.
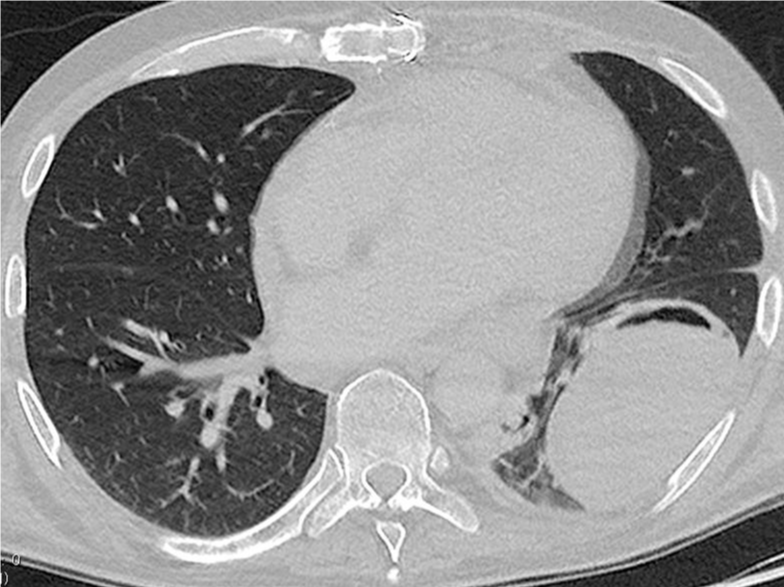
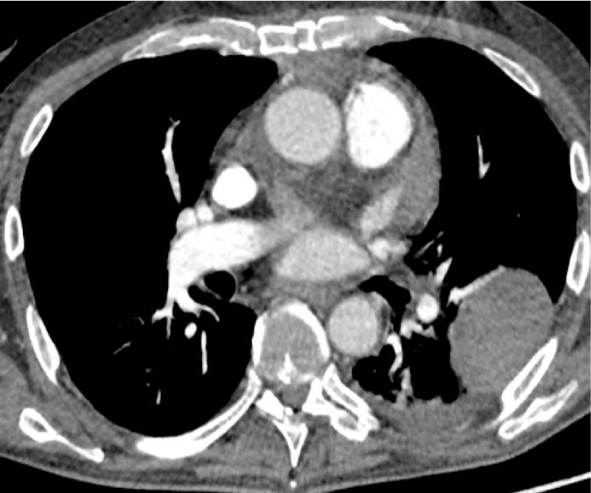
Figures 1 and 2 are the Chest CT performed prior to left lower lobectomy.
Figure 1: Chest CT, lung window. A round shaped mass is visible in the left lower lobe with wide pleural contact; along the ventral margin there is an air crescent. Angioinvasive aspergillosis generally presents as a pulmonary round mass and the “air crescent sign” is frequently seen in recovering invasive pulmonary aspergillosis (50%) [1]. The lesion presents imaging features very suggestive of aspergillosis.
Figure 2: Chest CT, mediastinal window.The pulmonary artery shows no filling defect; the mass appears as a round, solid and homogeneously hypovascular lesion. None of these features is coherent with the classic aspect of a pulmonary infarct (wedge shaped and associated with a thrombus in the feeding vessel); while their absence is coherent with the diagnosis of angioinvasive aspergillosis [2].
KEY MESSAGE
Even if the lesion did not reveal to be a fungal lesion aspergilloma on definitive pathological examination, lung lobectomy was justified by the fact that the inferior lobe would have never recovered a normal function.
REFERENCES
- Franquet T, Müller NL, Giménez A, Guembe P, de La Torre J, et al. Spectrum of pulmonary aspergillosis: histologic, clinical, and radiologic findings. Radiographics. 2001; 21: 825-837. Ref.: https://goo.gl/yIgqMZ
- Bray TJ, Mortensen KH, Gopalan D. Multimodality imaging of pulmonary infarction. Eur J Radiol. 2014; 83: 2240-2254. Ref.: https://goo.gl/R8RTCr