More Information
Submitted: August 21, 2023 | Approved: September 01, 2023 | Published: September 04, 2023
How to cite this article: Chang HM, Su CI, Chang CT. CT-guided Retrograde Urography as a Diagnostic Tool for Post-kidney Transplantation Evaluation: A Case Report. J Clin Med Exp Images. 2023; 7: 004-006.
DOI: 10.29328/journal.jcmei.1001028
Copyright License: © 2023 Chang HM, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Kidney transplantation; Major urologic complications; Computed tomography urography
CT-guided Retrograde Urography as a Diagnostic Tool for Post-kidney Transplantation Evaluation: A Case Report
Han-Mei Chang1, Chan-I Su2 and Ching-Ting Chang2,3*
1Department of Medical Imaging, Kaohsiung Municipal Ta-Tung Hospital, Kaohsiung 80145, Taiwan
2Department of Medical Imaging, Kaohsiung Medical University Hospital, Kaohsiung 80708, Taiwan
2,3Department of Medical Imaging, Kaohsiung Medical University Gangshan Hospital, Kaohsiung 82060, Taiwan
*Address for Correspondence: Ching-Ting Chang, Department of Medical Imaging, Kaohsiung Medical University Gangshan Hospital, Kaohsiung 82060, Taiwan, Email: [email protected]
The vast majority of urological complications occur at the ureterovesical junction and usually occur early after transplantation. The aim of this study is to enhance the quality of medical care provided to patients who undergo kidney transplantation. Cystography was conducted on renal transplant recipients utilizing computed tomography. The utilization of changes in the patient’s position and reconstructed images of the bladder can serve as a diagnostic tool to assess the normal functioning of the urinary tract system subsequent to kidney transplantation. To ensure adequate filling of the bladder and ureter, it is necessary to introduce varying amounts of contrast medium through the urinary catheter into these structures. This diagnostic procedure aims to verify the existence of stenosis or leakage occurring at the vesicoureteral junction. The evaluation and diagnosis of urinary tract problems subsequent to kidney transplantation can be effectively conducted. Furthermore, it has the potential to mitigate the adverse effects and alleviate the strain on the renal system resulting from the administration of contrast agents in computed tomography urography. CT-guided cystography can enhance the medical quality and comfort of Kidney transplantation patients.
Kidney transplantation (KTX) is widely recognized as the most efficacious therapeutic intervention for individuals afflicted with chronic kidney disease [1]. Can offer patients diagnosed with end-stage renal disease superior long-term survival rates and improved quality of life compared to maintenance hemodialysis. Major urologic complications (MUCs) are associated with increased morbidity and graft loss following KTX, particularly after episodes of rejection [2,3]. MUCs are a frequently observed complication following KTX. MUCs occur in approximately 9% of kidney transplants [4]. MUCs were defined as instances of urinary leakage, ureteral stricture, bladder outlet obstruction (BOO) (internal and external), graft stones, and vesicoureteral reflux [5-7]. Among them, the ureterovesical stricture is due to technical errors or ureteral blood vessels.
MUCs after KTX will cause complications in patients and endanger the function of the transplanted kidney. The vast majority of urological complications occur at the ureterovesical junction (UVJ) and usually occur early after transplantation [8,9].
Early detection and treatment of BOO is essential for maintaining long-term graft function. Indeed, adequate long-term graft function depends on low-pressure urine storage and effective bladder emptying [10,11]. In the case report, cystography was performed using computerized tomography (CT) to diagnose the normalcy of the urinary tract system after KTX. The patient’s position change and reconstructed images were utilized for this purpose.
A 57-year-old male patient with a medical history of recurrent ureteral obstruction and hydronephrosis underwent ureteric reconstruction and transplantation of the native ureter into the transplanted kidney.
CT cystography is a modified form of the conventional fluoroscopic cystogram. In contrast to CT urography, where anterograde opacification of the urinary collecting system is used, retrograde instillation of contrast into the patient’s bladder is employed, followed by imaging of the pelvis using CT.
The patient experienced acute tubular necrosis, acute rejection, and the presence of a residual thrombus within one week after KTX. Despite the placement of prophylactic ureteral stents post-surgery and the removal of the thrombus through cystoscopy, the observed urine flow did not meet the anticipated levels. This raised concerns regarding the possibility of UVJ stenosis or leakage. As a result, a consultation was made with the radiology department to conduct CT cystography.
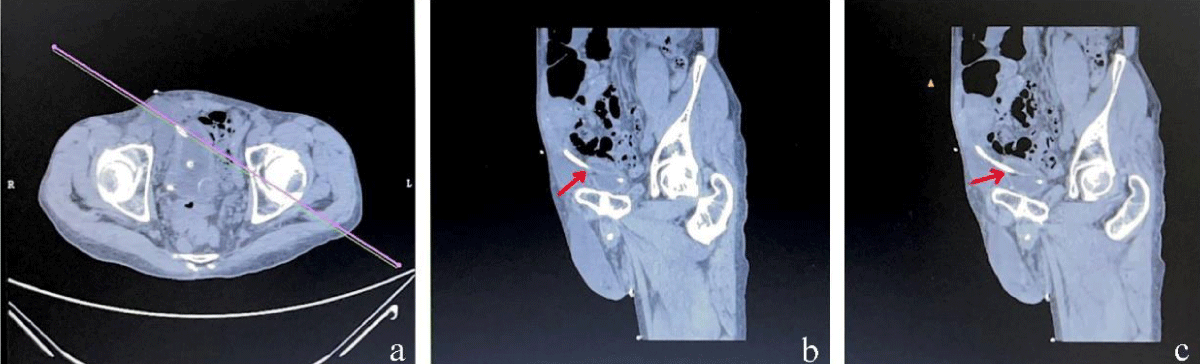
Radiologists utilized CT imaging with the Philips Brilliance 64-slice scanner to perform cystography. First, a reconstructed coronal plane image along the UVJ was obtained prior to contrast injection, as depicted in Figure 1. Subsequently, a dilute solution of iodinated contrast agent (ULTRAVIST®) was perfused through the urinary catheters. The ratio of iodinated contrast (300 mgI/mL) to water is 1:1.5. To assess the presence of stenosis or leakage at the UVJ and the smoothness of the ureteral stent and normal drainage, the following procedure was performed. A total of 160ml of fluid, divided into three equal portions of 60ml, 60ml, and 40ml, was used to fill the bladder and the ureter. The patient was positioned in three different ways: lying flat, lying oblique, and lying on the right side. Changes in angles were observed to confirm the presence of stenosis or leakage at the UVJ and to assess the smoothness of the ureteral stent and normal drainage.
Figure 1: (a) A reconstructed coronal plane image was obtained at the UVJ without the use of contrast injection. (b)(c) Acquire an image of the UVJ.
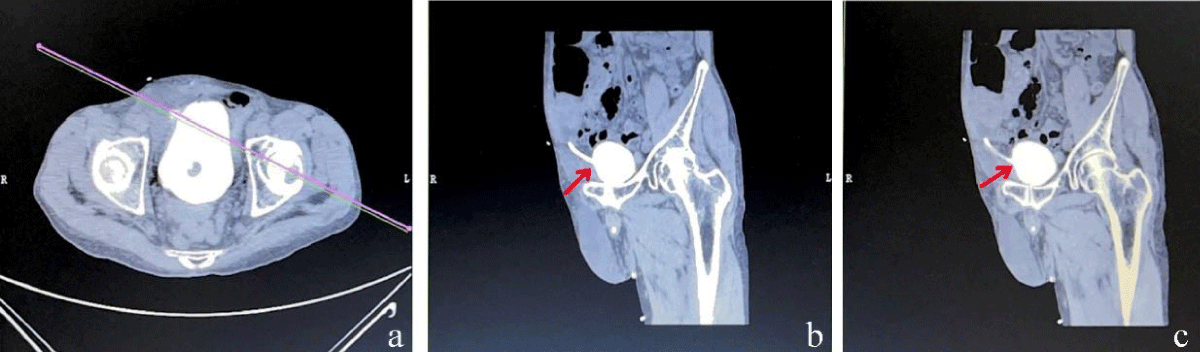
A contrast medium of 60mL was retrogradely administered through the urinary catheters into the bladder and ureter in order to enhance visualization of the stricture of the UVJ, as depicted in Figure 2.
Figure 2: (a) A reconstructed coronal plane image was obtained at the UVJ following contrast injection. (b)(c) The stricture of the UVJ is clearly observable.
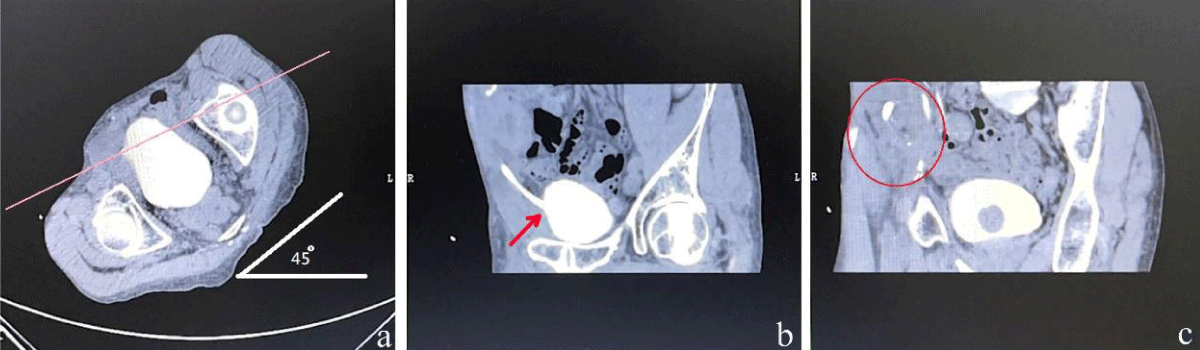
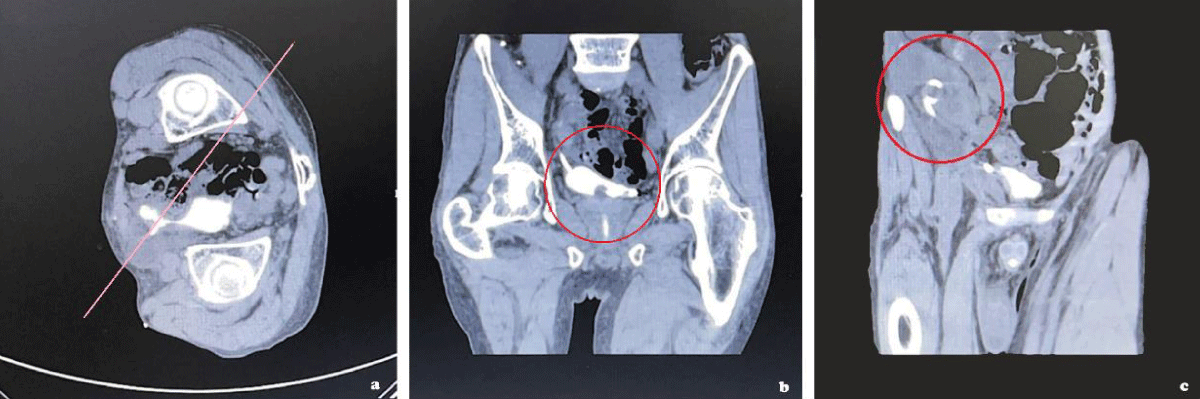
The patient’s left side should be elevated by 45 degrees, followed by the injection of 60mL of contrast medium to fill the bladder and ureter. This procedure allows for a clear observation of the narrowness of the UVJ, as depicted in Figure 3.
Figure 3: (a) The patient's left side was elevated by 45 degrees. (b) Demonstrate the UVJ more prominently. (c) Backflow of contrast agent into the transplanted kidney. (Indicated by the red circle).
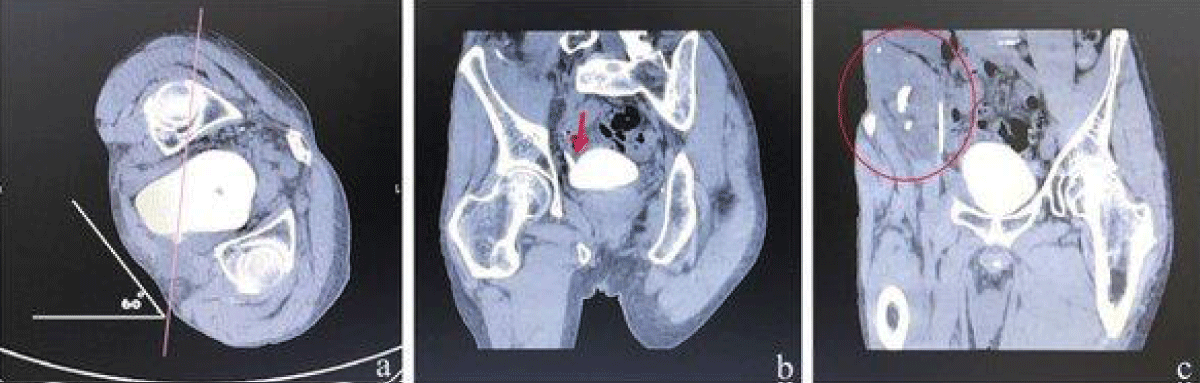
The patient’s position was altered to a prone position on the table, with the left side elevated by 60 degrees, while simultaneously administering a continuous infusion of 60mL of contrast medium. It can be observed from Figure 4 that the contrast medium has been administered to the renal pelvis of the transplanted kidney.
Figure 4: (a) Position the patient in a prone position, with a 60-degree inclination on the lower right side and upper left side. (b) The UVJ is clearly evident. (c) Retrograde flow of the contrast agent into the transplanted kidney. (Indicated by the red circle).
Following the excretion of the contrast medium from the bladder, a notable decrease in the volume of the contrast medium was observed in both the renal pelvis and bladder. This observation provides empirical evidence that demonstrates the functional adequacy of the urinary system following KTX, as depicted in Figure 5.
Figure 5: ((a) The patient was positioned in a right lateral posture subsequent to the introduction of the contrast agent into the bladder. (b)(c) A notable reduction in the concentration of the contrast agent was observed in both the bladder and renal pelvis exhibited a significant decrease (indicated by the red circle).
The bladder is fully filled with a retrograde contrast agent infusion, extending through the ureteral stent and reaching the transplanted renal pelvis. After implementing adjustments in body position and conducting image reconstruction, it can be ascertained that there is no evidence of leakage at the anastomosis site between the bladder and ureter. Additionally, the drainage function of the ureteral stent appears to be functioning normally.
One month later, the patient’s daily urine output was 1000-1300 mL, and he experienced nocturia 3-4 times per night. Two weeks later, the double-J stent was removed through cystoscopic retrograde pyelography, and the patient was able to resume a normal life.
Urinary tract system examinations are commonly performed utilizing a range of diagnostic techniques, such as intravenous urography (IVU), computed tomography urography (CTU) with contrast agent administration, cystoscopy, and retrograde pyelography (RP).
Compared to CT-guided cystography, IVU exhibits a lengthier examination duration and lacks the capability to capture images from multiple angles. Cystoscopy, despite its relative ease of execution, can induce pain and discomfort in patients and is associated with potential risks such as urinary tract infection or bleeding [12,13]. On the contrary, CTU necessitates the administration of a greater contrast dosage, which could potentially place an additional burden on KTX postoperatively and may not yield urinary tract images in a timely manner [14,15].
However, this case is not representative of all transplant recipients, as it is well-known that UVJ anastomosis methods are different.
Prompt diagnosis and treatment are essential in cases of renal transplant obstruction. Once the presence of ureteric obstruction is confirmed or strongly suspected, it is imperative to promptly initiate urinary diversion in order to mitigate potential kidney damage. Once renal function has shown improvement, the medical team proceeds with the definitive treatment of the obstruction in the ureter.
CT-guided cystography, utilizing CT guidance, offers the potential to integrate the benefits of the aforementioned examinations. This technique allows for the effective evaluation and diagnosis of urinary tract issues following KTX, while also mitigating the potential harm associated with contrast media injection during CTU and reducing the risks associated with invasive examinations. Consequently, the implementation of CT-guided cystography can significantly enhance the overall medical quality of KTX patients.
- Kumar S, Ameli-Renani S, Hakim A, Jeon JH, Shrivastava S, Patel U. Ureteral obstruction following renal transplantation: causes, diagnosis and management. Br J Radiol. 2014 Dec;87(1044):20140169. doi: 10.1259/bjr.20140169. Epub 2014 Oct 6. PMID: 25284426; PMCID: PMC4243200.
- Nino-Torres L, Garcia-Lopez A, Patino-Jaramillo N, Giron-Luque F, Nino-Murcia A. Risk Factors for Urologic Complications After Kidney Transplantation and Impact in Graft Survival. Res Rep Urol. 2022 Sep 28;14:327-337. doi: 10.2147/RRU.S371851. PMID: 36196091; PMCID: PMC9527029.
- Gupta R, Woo K, Yi JA. Epidemiology of end-stage kidney disease. Semin Vasc Surg. 2021 Mar;34(1):71-78. doi: 10.1053/j.semvascsurg.2021.02.010. Epub 2021 Feb 4. PMID: 33757639; PMCID: PMC8177747.
- Duty BD, Barry JM. Diagnosis and management of ureteral complications following renal transplantation. Asian J Urol. 2015 Oct;2(4):202-207. doi: 10.1016/j.ajur.2015.08.002. Epub 2015 Aug 24. PMID: 29264146; PMCID: PMC5730752.
- Nie Z, Zhang K, Huo W, Li Q, Zhu F, Jin F. Comparison of urological complications with primary ureteroureterostomy versus conventional ureteroneocystostomy. Clin Transplant. 2010 Sep-Oct;24(5):615-9. doi: 10.1111/j.1399-0012.2009.01134.x. PMID: 19925475.
- Bruintjes MHD, d'Ancona FCH, Zhu X, Hoitsma AJ, Warlé MC. An Update on Early Urological Complications in Kidney Transplantation: A National Cohort Study. Ann Transplant. 2019 Dec 3;24:617-624. doi: 10.12659/AOT.920086. PMID: 31792196; PMCID: PMC6909919.
- Sarıer M, Duman İ, Demir M, Yüksel Y, Emek M, Kukul E. The outcomes of transurethral incision/resection of the prostate (TUIP/TURP) performed early after renal transplantation. Turk J Urol. 2018 Mar;44(2):172-177. doi: 10.5152/tud.2018.98404. Epub 2018 Mar 1. PMID: 29511589; PMCID: PMC5832381.
- Ostrowski M, Włodarczyk Z, Wesołowski T, Gracz H, Sluzar T, Sieńko J, Lubikowski J, Bohatyrewicz R. Influence of ureterovesical anastomosis technique on the incidence of vesicoureteral reflux in renal transplant recipients. Ann Transplant. 1999;4(1):54-8. PMID: 10850602.
- Rahnemai-Azar AA, Gilchrist BF, Kayler LK. Independent risk factors for early urologic complications after kidney transplantation. Clin Transplant. 2015 May;29(5):403-8. doi: 10.1111/ctr.12530. Epub 2015 Mar 6. PMID: 25683841.
- Sarier M, Yayar O, Yavuz A, Turgut H, Kukul E. Update on the Management of Urological Problems Following Kidney Transplantation. Urol Int. 2021;105(7-8):541-547. doi: 10.1159/000512885. Epub 2021 Jan 28. PMID: 33508852.
- Gökçe AM, Kaya C, Kara VM, Ozel L, Ruhi C, Titiz MI. Effects of Urethral Stricture on Allografts in Kidney Transplantation. Transplant Proc. 2015 Jun;47(5):1336-9. doi: 10.1016/j.transproceed.2015.04.072. PMID: 26093713.
- Engelsgjerd JS, Deibert CM. Cystoscopy. 2023 Apr 10. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 29630232.
- Ellerkmann RM, Dunn JS, McBride AW, Kummer LG, Melick CF, Bent AE, Blomquist JL. A comparison of anticipated pain before and pain rating after the procedure in patients who undergo cystourethroscopy. Am J Obstet Gynecol. 2003 Jul;189(1):66-9. doi: 10.1067/mob.2003.377. PMID: 12861140.
- Park MS, Ha HI, Ahn JH, Lee IJ, Lim HK. Reducing contrast-agent volume and radiation dose in CT with 90-kVp tube voltage, high tube current modulation, and advanced iteration algorithm. PLoS One. 2023 Jun 15;18(6):e0287214. doi: 10.1371/journal.pone.0287214. PMID: 37319309; PMCID: PMC10270572.
- Davenport MS, Khalatbari S, Dillman JR, Cohan RH, Caoili EM, Ellis JH. Contrast material-induced nephrotoxicity and intravenous low-osmolality iodinated contrast material. Radiology. 2013 Apr;267(1):94-105. doi: 10.1148/radiol.12121394. Epub 2013 Jan 29. PMID: 23360737; PMCID: PMC3606541.